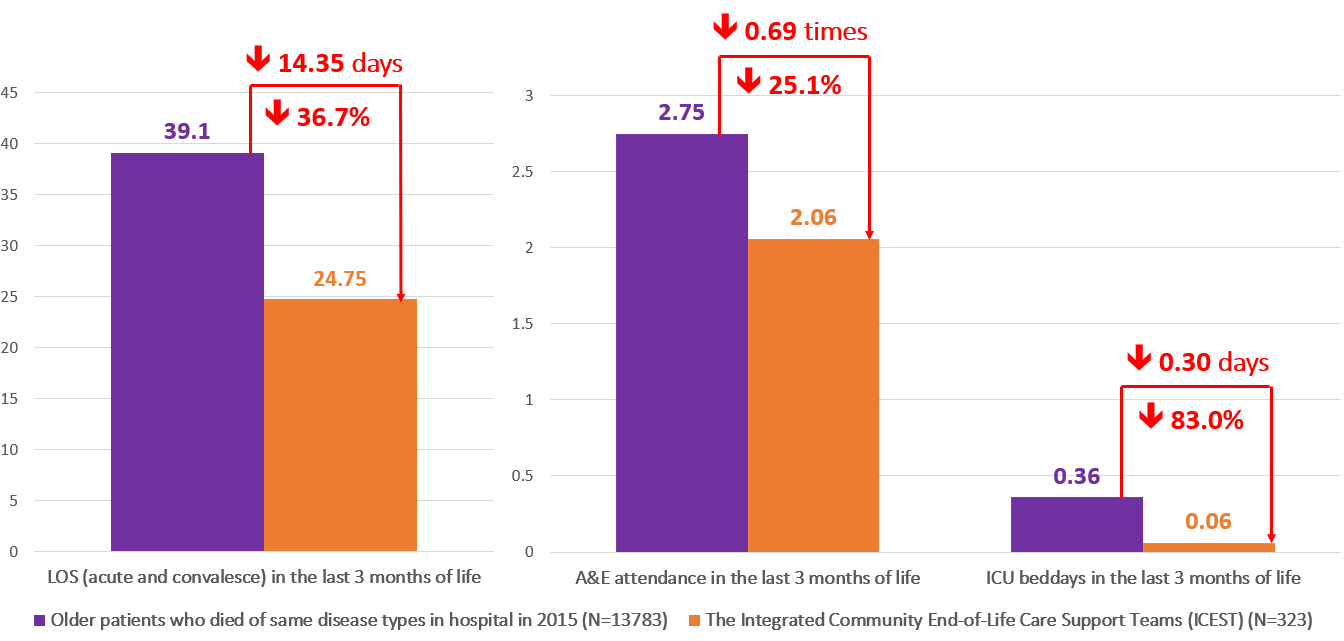
Projecting this finding to 1 410 patients served by the four NGOs, the programmes would have helped spared 20 234 hospital bed days, 423 ICU beddays, and 973 A&E attendances to other needy patients. Taking the cost of these medical service into consideration, the programmes have also helped save 134 million medical costs
Evaluation on the Integrated community End-of-Life Care Support Teams (ICESTs)
Beneficiaries
The EoLC programmes delivered by four NGOs had benefited altogether 1 410 patients and their family caregivers between 2019 and 2021. These patients comprised of 51.6% cancer patients, 18.9% with renal disease, 6.1% with lung disease, and the remaining consists of patients with various non-cancer conditions.
Methodology
For the methodology of evaluating the outcomes and impacts of the community-based EoLC programmes, please refer to Phase I methodology:
In addition, different from the quantitative evaluation with “community partners” in Phase I, the University of Hong Kong conducted individual in-depth interviews with patients and family caregivers who received services between 2019 to 2021. This qualitative study aims at exploring the satisfaction levels and view of service recipients regarding the service implementation and overall effectiveness of JCECC EoLC services. A total of 7 patients and 10 caregivers were interviewed.
Achievements
Significant Improvements on Quality of Life in Patient
A total of 406 patients completed the assessments at service intake and 3 months after services (figure 1). Assessed patients reported 26.8% reduction of physical symptoms, 38.3% reduction of depressive symptoms, and 35.1% reduction of anxiety. Additionally, their information needs and practical problems greatly reduced by 42.8% and 49.5% respectively. Meanwhile, patients also reported 33.4% reduction in spiritual distresses, 29.8% reduction in family conflicts and 27.2% of social distress. These changes were statistically significant (p <.001).
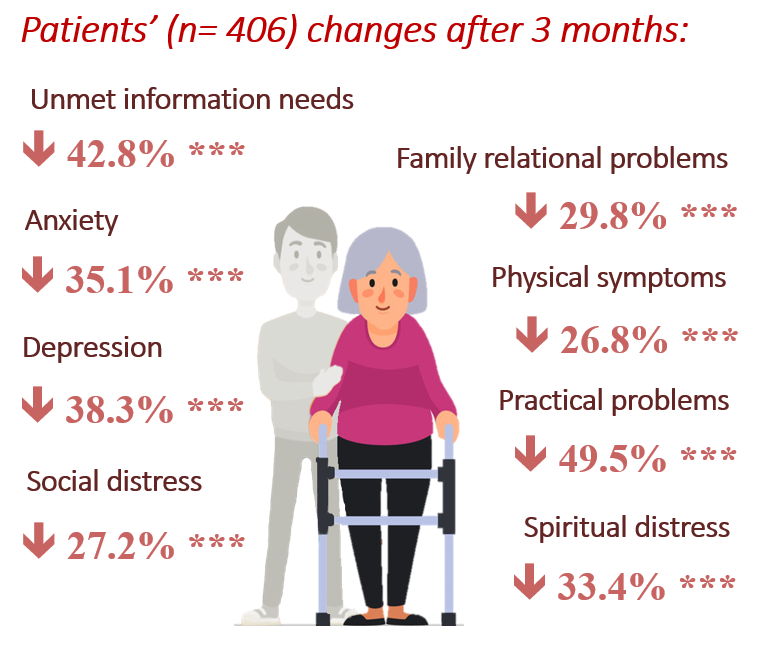
. Patients’ changes in quality of life 3 months after services
Significant Improvements on Caregiving Stress and Emotions in Family Caregivers
A total of 343 family caregivers completed the assessments at service intake and 3 months after services (figure 2). Assessed caregivers reported 23.5% reduction in caregiver strain, 35.2% reduction in depressive symptoms, and 21.3% reduction in anxiety. Caregivers reported 11.8% reduction in distress when facing patients’ medical decision and 14.5% reduction in anxiety when patients’ condition deteriorates. These changes were statistically significant (p <.001). Moreover, among 352 bereaved family caregivers who were assessed two months after the death of patients, 95.7% reported low level of complicated grief.
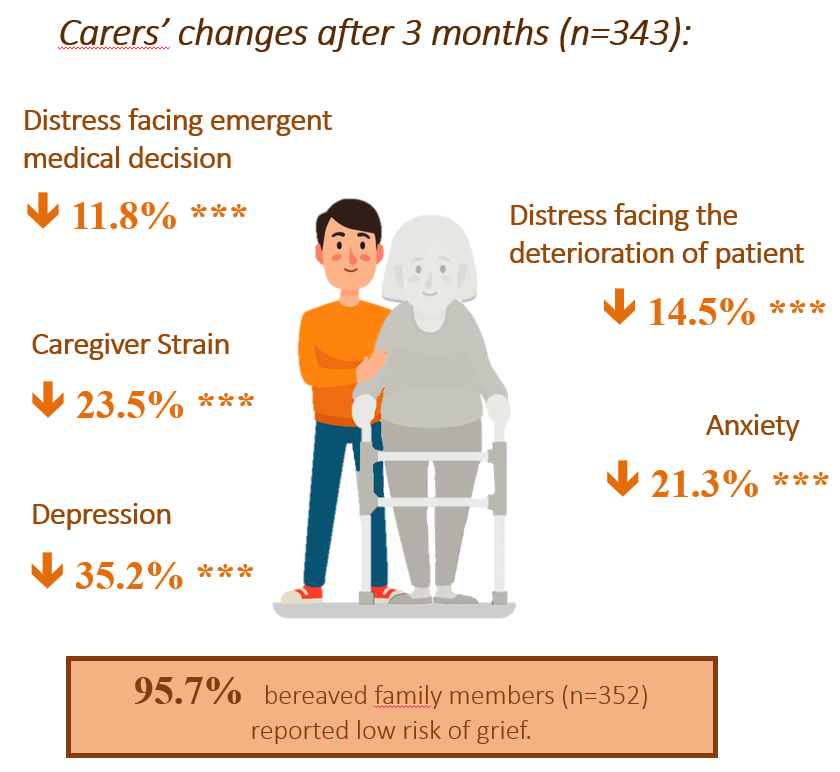
Carers’ changes in quality of life 3 months after services.
Reduced Unnecessary Medical Service Utilisation
Regarding service impact on medical service utilisation in the last 6 months of life, retrievable data from 323 deceased patients suggested that the programme patients had 14.35 fewer hospital beddays, 0.69 fewer A&E attendances, and 0.30 fewer ICU beddays than EoL patients in general (figure 3). This result supports the effectiveness of the community-based EoLC programmes in helping patients to avoid unnecessary hospitalisation and stay home longer.
Cost-benefit

Offered 20 234 hospital beddays for other needy patients

Offered 423 ICU beddays for other needy patients

Reduced 249 A&E visits
HKD$133 861 820
Social return on Investment (SROI) analysis was further conducted on 3 ICESTs1 over the 3 years. Findings suggested that $1 HK invested in ICEST could generate $3.58 HK of social values in return, suggesting that the ICEST was cost-effective

輸入HK$32.3百萬的輸入
輸出患者+照顧者+義工的成效: HK$13.25百萬+減少的醫療服務使用率: HK$102.1百萬 = 總輸出: HK$115.4百萬
High Service Satisfaction
Majority of the surveyed patients and family caregivers reported highly satisfied experience with the services. Among 120 surveyed patients and 249 family caregivers, 93.8% and 96.0% respectively express high level of overall satisfaction towards the services (7/10 or higher). Moreover, 91.1% of surveyed patients reported that their preferences on the care plan have been respected by the service team; while 90.2% of surveyed caregivers reported that the service team enabled them to effectively take care of patients’ daily life at home environment (7/10 or higher).
Learnings in phase I and way forward in phase II
Compared to Phase I, The programmes not only effectively improved the quality of life of patients and their caregivers from physical, mental, social and spiritual aspects, but unnecessary medical service utilisation among patients, allowing them to be taken care at home. More importantly, the programmes also resulted in significant savings in medical Furthermore, the programmes provide a satisfying experience for the majority of patients and caregivers, which patients found to be respectful to their care decision while effectively supported caregivers take care patients at home.
Based on the findings from these 6 years, effective service components were extracted to develop a unified service model – the Integrated Community End-of-Life Care Support Teams, and to improve the services according to the needs of patients and caregivers.