Extrapolating this finding to 502 residents served by the HKAG programme, it is estimated that the programme has helped spared 8,850 hospital beddays, 236 times of A&E attendance and 141 ICU beddays to other needy patients. Taking the cost of these medical services into consideration, the EoLC programme in RCHEs have also helped save 57.1 million medical costs.
Evaluation of EoLC in Residential Care Home for the Elderly (RCHEs)
Beneficiaries
The HKAG programme aims at upskilling RCHEs staff to provide EoLC. Residents in their end of life are the end users of the programme. Hence, the programme’s impacts on EoL residents were also evaluated. Particularly, we are interested in the programme’s effectiveness on improving the quality of life and reducing unnecessary medical service utilisation of EoL residents in the RCHEs. By the end of December 2021, the HKAG programme has served 502 residents and their respective family caregivers between 2019 and 2021.
Methodology
Residents and their primary family caregivers were assessed using structured and standardised measurements. For residents, their physical symptoms, depression, anxiety and practical concerns were assessed by “The Integrated Palliative Care Outcome Scale” (IPOS) at service intake, one month after service, and three months after the service respectively. For family caregivers, their emotional symptoms were assessed at service intake and two months after the patient’s death, while level of grief was assessed by the Chinese “Inventory of Complicated Grief” (ICG) only at two months after the patient’s death. Apart from clinical assessment, family caregivers were also surveyed for their satisfaction towards services by the research team from the University of Hong Kong.
Regarding service impact, the medical service utilisation in the last 6 months in life of deceased patients in the HKAG programme was compared to that of the deceased end-of-life patients in 2015 in Hong Kong who had a principal diagnosis of cancer, COPD, congestive heart failure, end-stage renal diseases, motor neuron disease, and Parkinson’s disease. These data were retrieved from the Central Panel on Administrative Assessment of External Data (CPAA) of Hospital Authority in a clinical data mining (CDM).
In addition, the University of Hong Kong also conducted focus groups with managerial and professional staff and individual interviews with supporting care staff in RCHEs. This qualitative study aims at exploring the view of service implementer regarding the service implementation and overall effectiveness of JCECC EoLC services. A total of 3 focus groups and 7 interviews were carried out.
Achievements
Significant Improvements on Quality of Life in Residents
A total of 323 residents completed the assessments at service intake and 3 months after service (figure 1). Assessed residents reported 28.4% reduction of pain symptoms, 22.3% reduction of shortness of breath, 38.6% reduction of difficulty in sleeping, and 12.8% of weakness. Additionally, their anxiety and practical problems also reduced by 19.6% and 14.4% respectively. These changes were statistically significant (p <.05).
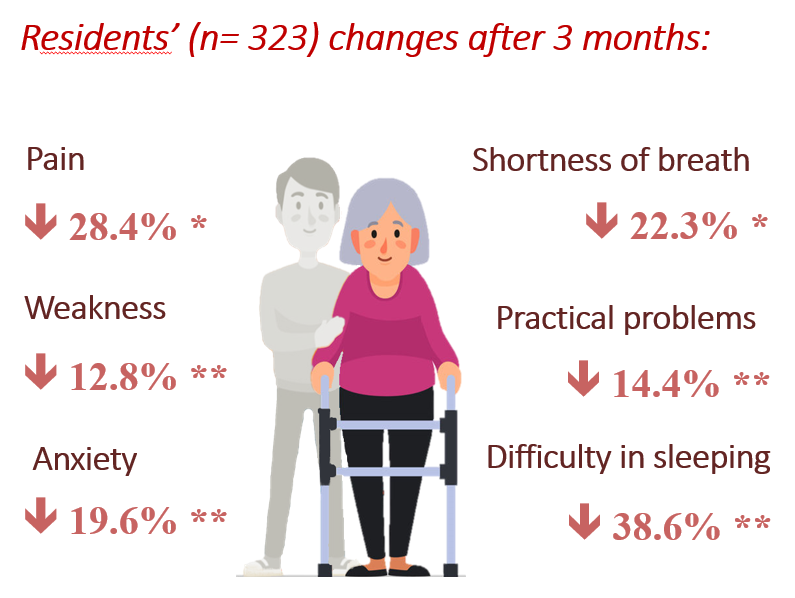
Residents’ changes in quality of life 3 months after services
Significant Improvements on Stress and Emotions in Family Caregivers
A total of 271 family caregivers completed the assessments at service intake and 2 months after the resident’s death (figure 2). Assessed caregivers reported 48.2% reduction of distress when facing emergent medical decision of their sick family member and 50.5% reduction of anxiety when the patient’s health condition deteriorates. Moreover, their depression also greatly reduced by 83.5%. These changes were statistically significant (p <.001). Moreover, all bereaved family caregivers who being assessed two months after the death of patients (n=273) reported low level of complicated grief.
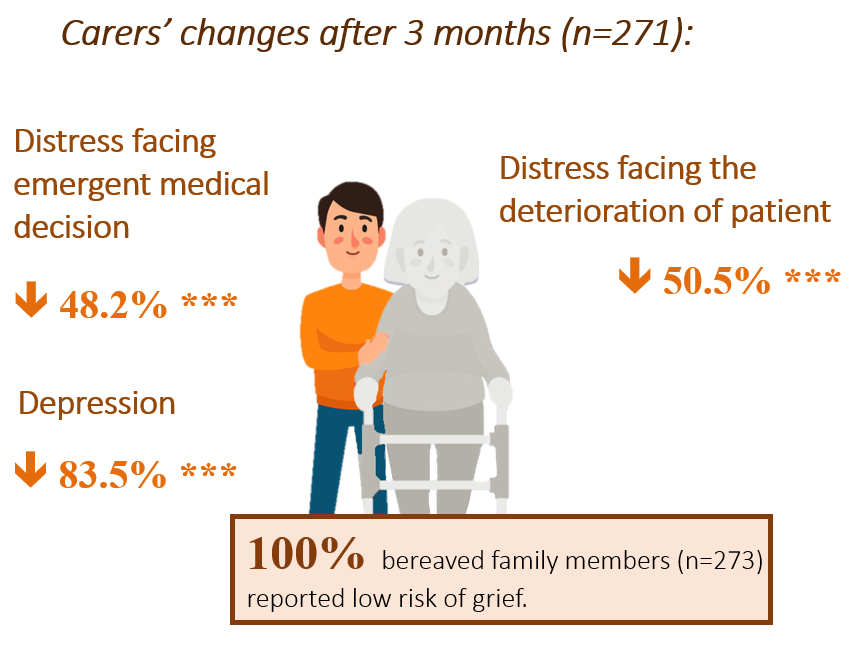
Carers’ changes in quality of life 2 months after the resident’s death.
Reduced Unnecessary Medical Service Utilisation
Regarding service impact on medical service utilisation in retrievable data from 134 deceased residents suggested that deceased residents in the HKAG programme had 17.63 fewer hospital beddays, 0.47 fewer A&E attendances and 0.28 days fewer ICU beddays than EoL patients in general (figure 3). This result supports the effectiveness of the programme in helping residents to avoid unnecessary hospitalisation and stay longer in familiar environment – the RCHEs.


Offered 8 850 hospital beddays for other needy patients

Offered 141 ICU beddays for other needy patients

Reduced 236 A&E visits
HKD$57, 128, 202

High Service Satisfaction
Majority of the surveyed family caregivers reported highly satisfied experience with the services. Among 86 family caregivers, 94.2% express high level of overall satisfaction towards the services (7/10 or higher).
Learnings in phase II and way forward in phase III
The EoLC programmes in RCHEs not only relieved both physical and emotional distress of EoL residents, but also reduced the strain and negative emotions in their respective caregivers. Meanwhile, these programmes also alleviated the torment to dying residents caused by repeated hospitalisation as well as greatly reduced medical expenses. In the coming four years, this model will be extended to more RCHEs to benefit more residents who have EoL issues and their caregivers.