Despite the COVID-19 pandemic between 2020 and 2021, the JCECC Project team had continued to offer public education via different kind of media to promote EoLC among the public, including newspaper columns, public education booklets and educational videos, public seminars, and an online learning platform for patients and family carers. Various public education activities were orchestrated surrounding three themes, namely “End-of-Life Decision Making (抉擇有時)” in 2019, “Communication (溝通有法)” and “Good Living/Good Dying (晚晴有你)”in 2020 and 2021. In particular, the Project collaborated with the Food and Health Bureau of the HKSAR Government, and the Hospital Authority to organise a public seminar series called “賽馬會安寧頌安寧照顧社區講座系列:晚期照顧抉擇您有Say” that attracted over 550 participants and supported the opinion gathering for the public consultation on the proposal for legislation of advance directives and dying in place. In addition, in response to the lockdown of the community support services during COVID-19, the Project team produced an electronic COVID-19 community resources guidebook for end-of-life patients and their family caregivers (“新型冠狀病毒病下的社區晚期病人照顧資源冊”) in a timely manner in June 2020, benefiting around 10,000 general public via our list of correspondence. To gauge the public awareness on and attitude towards EoLC and the changes during the same period, the same community wide phone survey that were carried out in the Phase I Projectwas conducted again at two time points in the Phase II Project.
Public Education
The Programme and Beneficiaries
Methodology
The Social Sciences Research Centre of the University of Hong Kong was commissioned to carry out this community-wide public phone survey. Residents in all districts of Hong Kong aged 18 above who spoke Cantonese, Putonghua or English would be randomly drawn to participate in the interview. The same survey was conducted twice in two separated time points: one between June and September, 2020, and another between June and September, 2021. In each wave, respondents were interviewed about their knowledge and attitude related to EoLC. There were 1 511 and 1 505 respondents in 2020 and 2021 respectively. The results in 2020 and 2021 were compared with the one conducted in 2018 to gauge the changes over time. Differences among years were tested using chi-square tests after controlling for demographics (gender, age, education, whether one has chronic illness, whether one’s family member(s) have chronic illness/terminal illness, whether one is currently taking care of family member(s) with chronic illness/terminal illness) factors. Bonferroni correction was also applied.
Key Finding
Knowledge
Overall, the surveyed respondents showed improved awareness on various important EoLC-related terms across years (Figure 1):
- Comparing the changes in percentage of respondents who have heard of EoLC-related terms across years, it was found that
- significantly more respondents have heard of palliative care (紓緩治療), hospice care (善終服務), DNACPR (不作心肺復甦術), and ACP (預設照顧計劃) across years. Comparing between 2018 and 2021, the percentages of increase for ACP, DNACPR, Palliative care, and hospice care were as high as 84.2%, 34.3%, 27.4%, and 9.4% respectively.
- Nevertheless, respondents who have heard of EoLC (安寧照顧) significantly dropped by 25.1% between 2018 and 2021 (from 39% in 2018 to 29.2% in 2021).
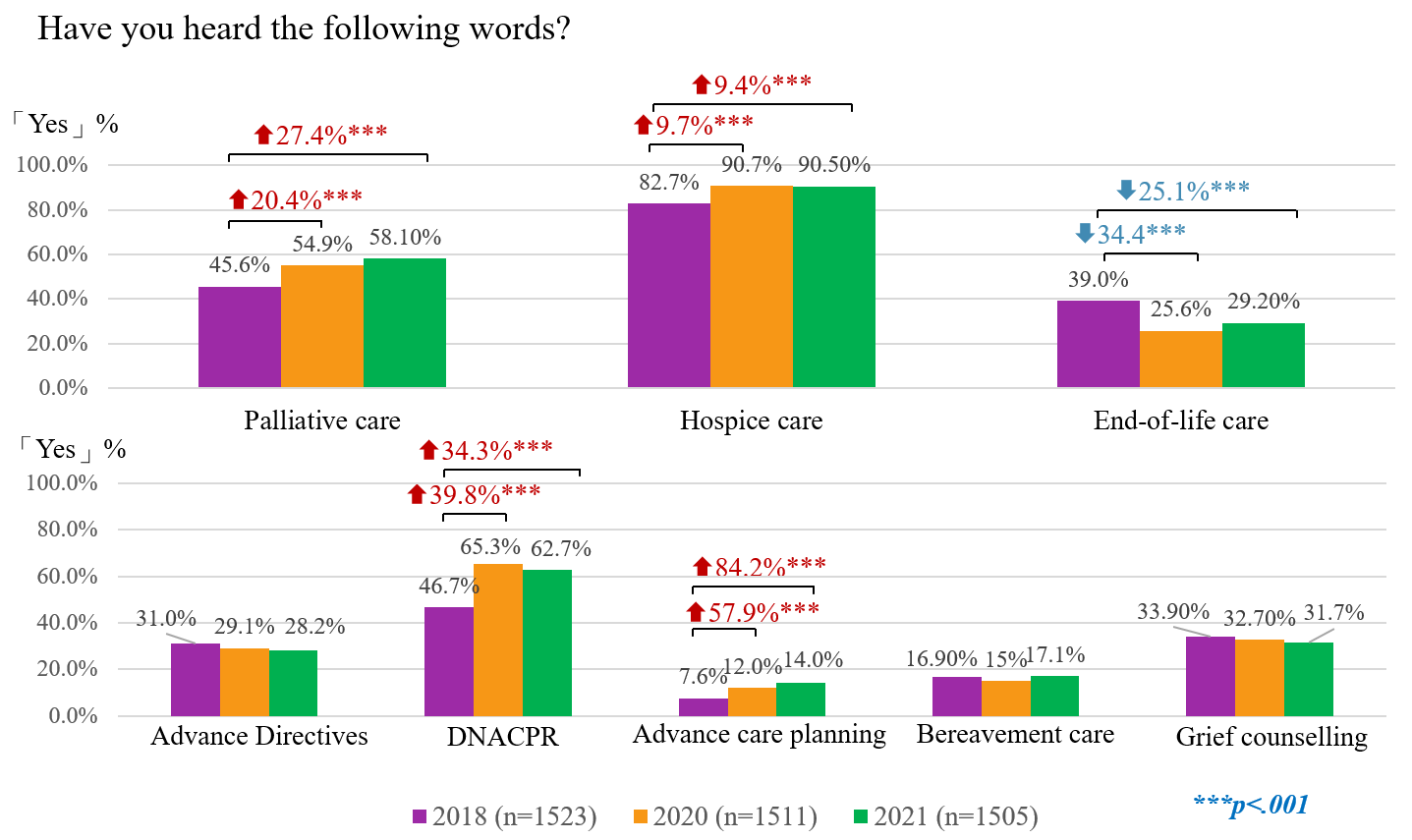
Figure 1. Comparison between 2018, 2020 and 2021 on hearing EoLC-related terms
Attitude
In all waves of survey, most survey respondents were open to discuss EoLC and death and dying issues. The responses of the survey respondents showed that they favoured an EoLC that encompasses self-involvement in decision making, making medical directives and care plan in advance, and prioritising quality of life over life-prolongation – which was in line with the principles of palliative and EoLC. Moreover, significant increase in the proportions of respondents who were open to discuss the EoLC topic, preferred treatments that emphasised quality of life instead of life-prolongation and considered to take advance directive (AD) and advance care planning (ACP) for themselves in future were observed either between the 2018 and 2020 waves or 2018 and 2021 waves of survey. In addition, surveyed respondents showed a preference on having different choices in regard of place of care and place of death. Especially, the percentages of respondents choosing domestic home or hospice centre as the most preferred place for death increased across year.
- Openness towards the EoLC Over the years, majority of the respondents reported being comfortable to discuss EoLC topic, ranging from 88.2% in 2018, 90.3% in 2021, to 92.2% in 2020 (Figure 2). A significant increase by 4.5% (p<.001) was found from 2018 to 2020.
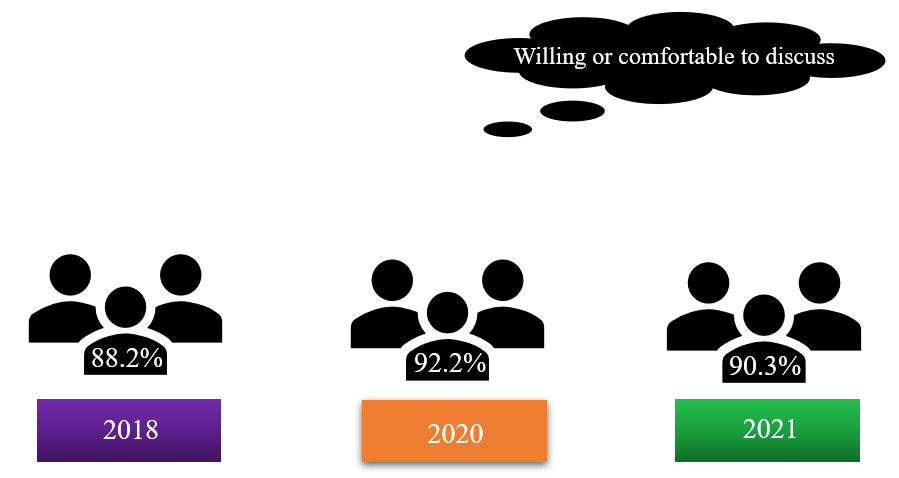
Figure 2. Openness towards talking about EoLC and death and dying
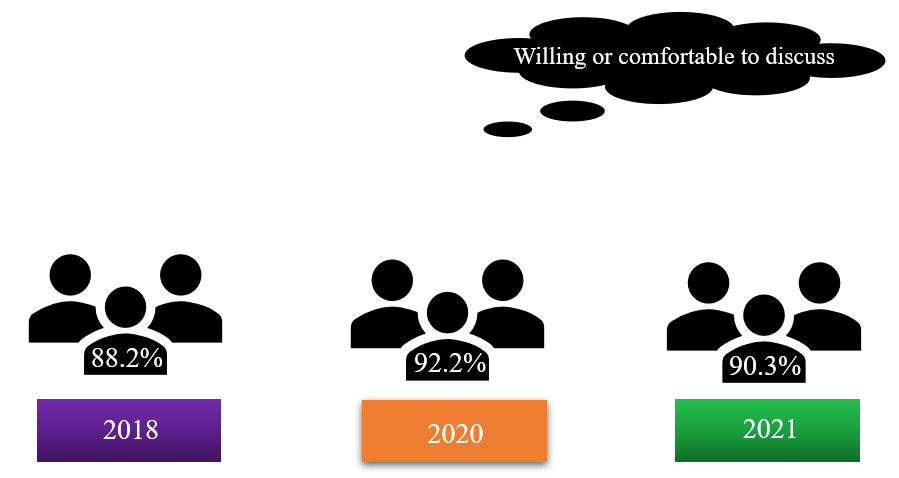
Figure 3. Final Medical Decision
- Preferred type of treatment. Under a hypothetical situation of last 6 months of life, respondents were asked whether they would choose treatments that may not prolong life but enhance quality of life or treatments that are life-prolonging but might incur discomfort. Results suggested that increasingly more respondents preferred treatments that emphasized quality of life instead of life-prolongation from 2018 to 2021, with this trend peaking in 2020. Those who opted for treatment emphasizing quality of life increased by 17.8% (p<.001) in 2020, and by 13.5% (p<.001) in 2021, as compared to 2018 (Figure 4). At the same time, those who chose life-prolonging treatments reduced significantly by 30.6% (p<.001) in 2020 and by 30.2% (p<.001) in 2021 compared with 2018.
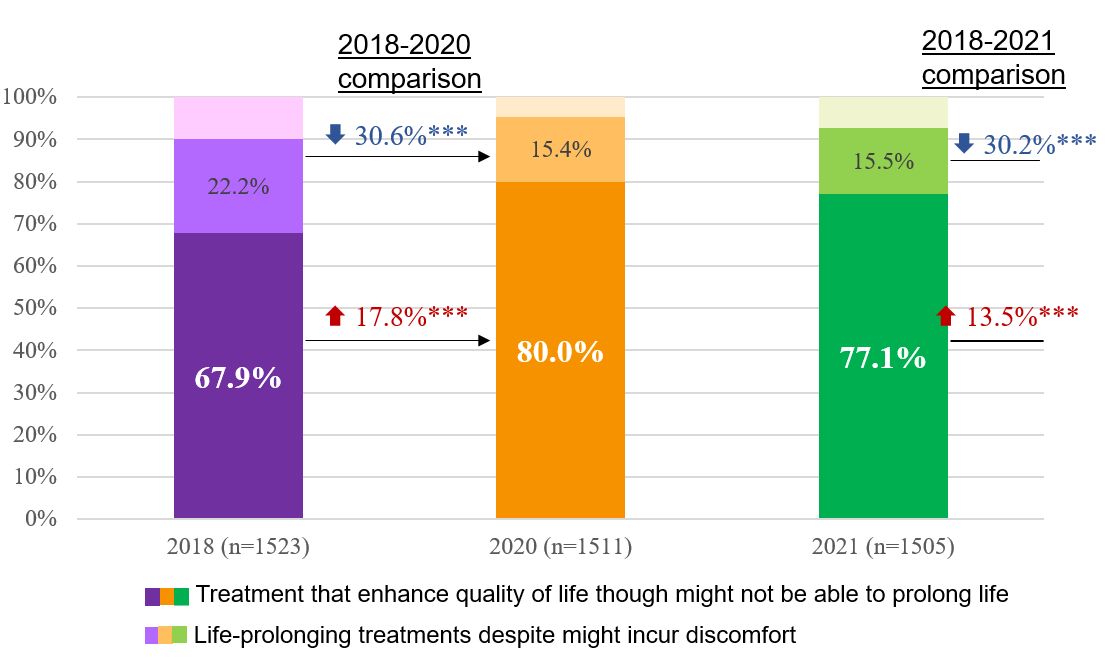
Figure 4. Preferred type of treatment
- Attitude towards conducting AD and ACP. The support towards conducting AD in future for oneself increased by 6.9% (p<.01) in 2020 when compared to 2018 (Figure 5). Moreover, more than 8 in 10 respondents in 2020 and 2021 supported the idea of conducting AD for oneself in future. Similarly, the proportion of support on conducting ACP significantly increased in 2020 and 2021 by 10.2% (p<.001) and 7.9% (p<.001) as compared to 2018 (Figure 5). Moreover, over eight in ten people express willingness to conduct AD and ACP for oneself in future in the 2020 and 2021 surveys.
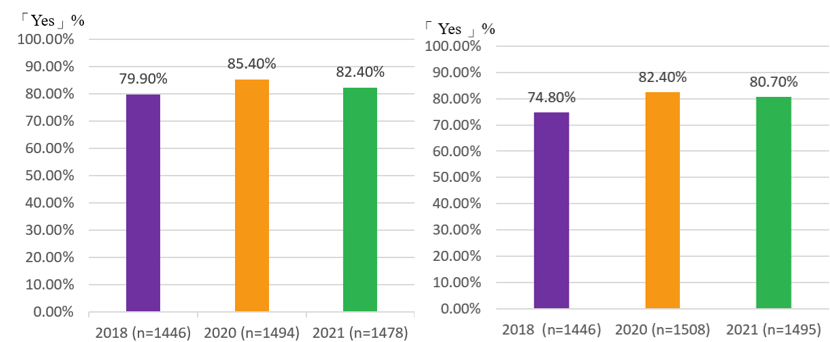
Figure 5. Attitudes towards conducting AD and ACP
- Preferred place for EoLC. Respondents were asked to choose their most preferred place of EoLC if they were under a hypothetical situation of last 6 months of life. Across years, domestic home is the most frequently opted place for care at the end of life (29% in 2020 and 28.2% in 2021), followed by infirmary (24.3% in 2020 and 25.8% in 2021), hospice centre (23.5% in 2020 and 20.7% in 2021), hospital (12.8% in 2020 and 14.4% in 2021), and finally elderly/nursing homes (8.4% in 2020 and 7.4% in 2021) (Figure 6). No significant changes were found between the two years.
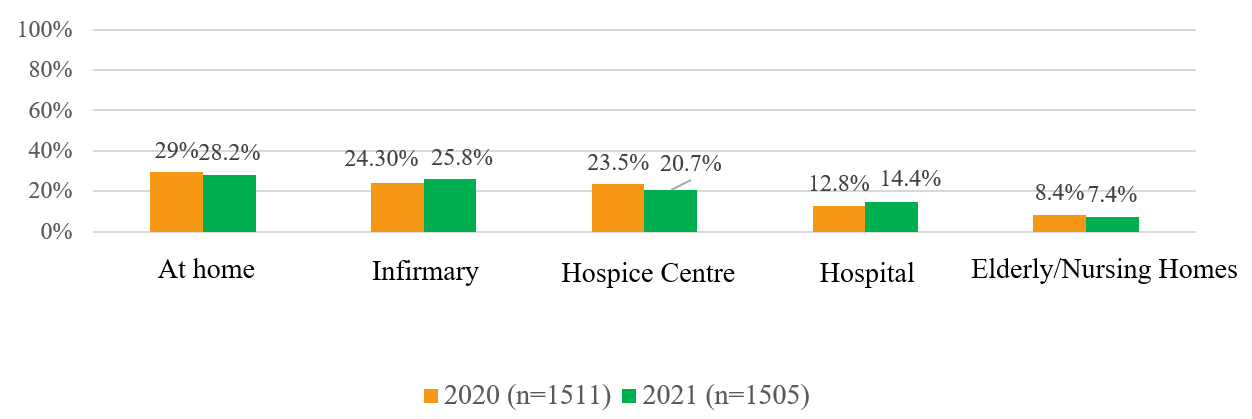
Figure 6. Most preferred place for EoLC across years
- Preferred place of Death. Respondents were asked to choose their most preferred place of death if they were under a hypothetical situation of last 6 months of life. In all years, hospital was the most frequently chosen place for death followed by domestic homes. However, the proportion of respondents choosing hospital reduced significantly across years while those choosing domestic home or infirmary/hospice centre increased significantly across years. At the same time, there was a significant reduction in proportion choosing elderly homes between 2018 and 2020. In 2021, around 5 out of 10 persons would choose hospital, 4 would chose home, and 1 would chose infirmary/hospice (Figure 7).
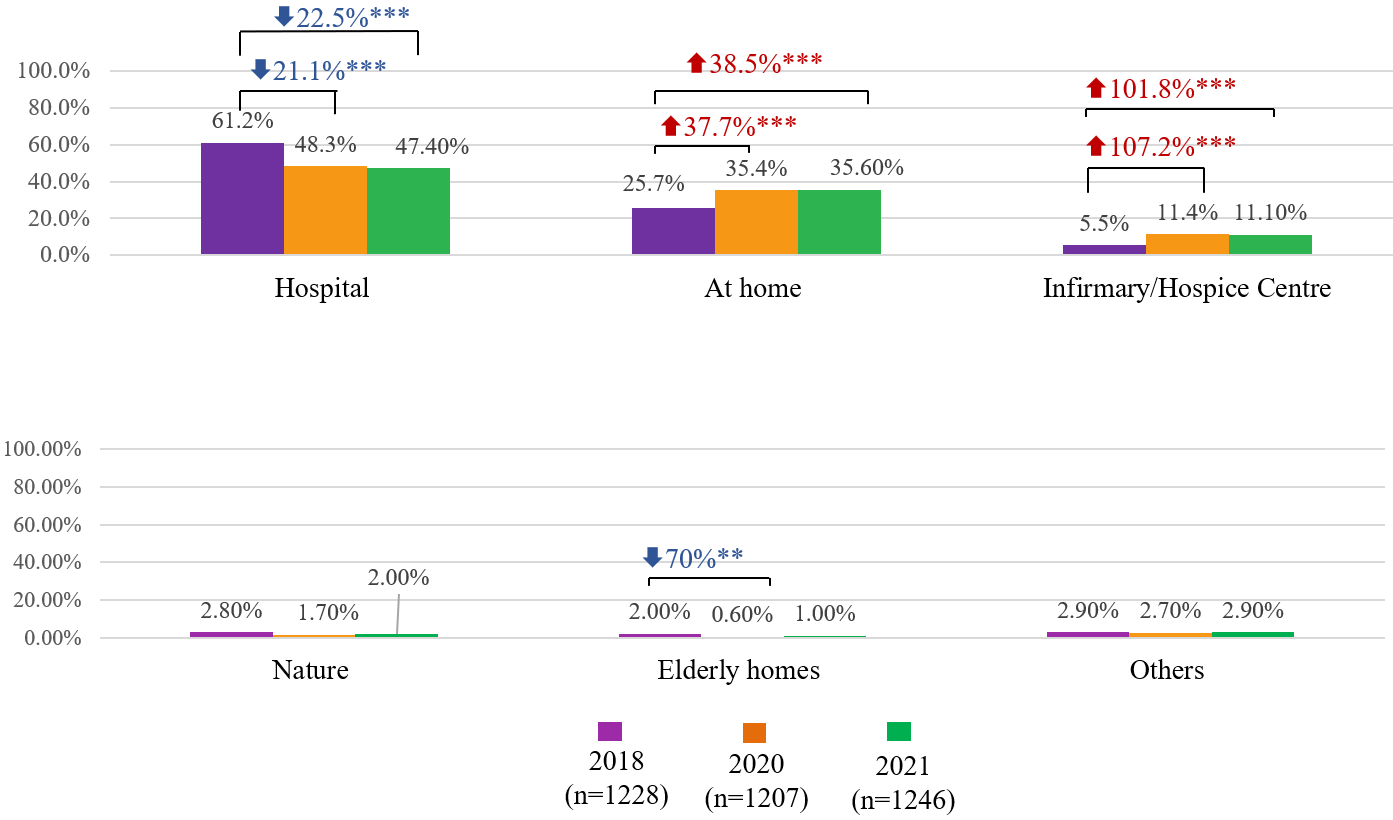
Figure 7. Most preferred place of death across year
Learnings in phase II and way forward in phase Ⅲ Project
- Compared with 2018, respondents’ awareness on EoLC-related terminologies improved in the 2020 and 2021 waves, in particular, the awareness towards the term “ACP” increased dramatically across years.
- Regarding the attitudes, the current findings showed that the respondents were open and ready for the discussion of topics related to EoLC and death and dying. Moreover, over three-fourth of respondents in all years showed preference on self-involvement in medical decision making, conducting ACP and AD, and choosing treatments emphasizing quality of life which are in line with the practices of EoLC. There were also increasing percentages of respondents choosing these EoLC-related practices across years. These all suggested high acceptance towards EoLC approach among the respondents.
- Respondents’ preference on place of EoLC and place of death in all three waves consistently showed that considerable respondents preferred community settings such as domestic home and elderly residential care homes apart from hospital, reflecting their needs and support for community-based EoLC. Probably due to the visitation restrictions in hospital during COVID-19 pandemic, the percentage of respondents in 2020 and 2021 who opted for home as a place for death increased substantially.
- The public has a favourable attitude and improving knowledge base on EoLC that are conducive to the further development of community EoLC. To further mobilise the general public to build a caring community for home-dwelling end-of-life patients and their families, public campaigns should be conducted in the phase III project to step up effort in engaging the general public into concrete actions, for instance, discussing EoLC, AD and ACP with their significant others. Tools and advice should also be offered to the general public to support them in these discussions.